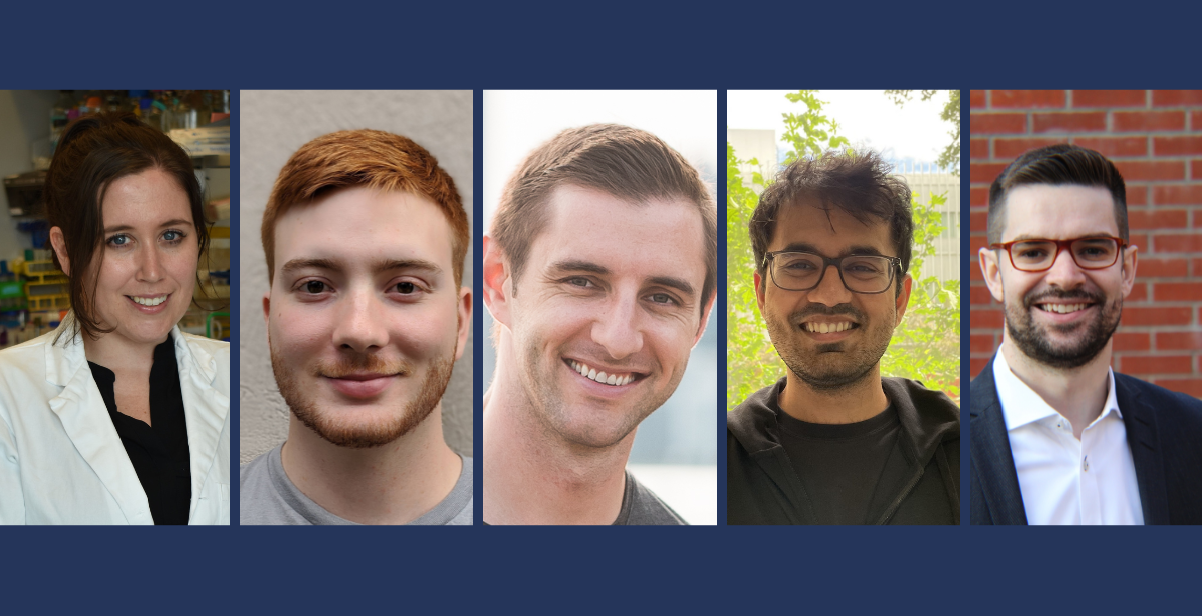
From left: Véronique Taylor, Duncan Carruthers-Lay, Marcus Dillon, Viplav Agarwal, Michael Fralick
November 28, 2024
By Sunitha Chari
As communities around the world marked World Antimicrobial Resistance (AMR) Awareness Week from November 18 to 24, 2024 we shine the spotlight on members of the Emerging and Pandemic Infections Consortium (EPIC) who are leading the fight against AMR.
These researchers are pioneering approaches that extend across different disciplines of basic and clinical research aimed at improving drug resistance monitoring and developing treatment strategies to lessen the AMR burden.
Patients in hospital settings are at a high risk of acquiring infections. This risk is highest for immunocompromised patients, such as premature babies whose immune systems have not fully developed. According to Michael Fralick, a clinician scientist at Sinai Health and an associate professor in the department of medicine at the University of Toronto’s Temerty Faculty of Medicine, premature babies are particularly vulnerable to developing blood stream infections during their stay in neonatal intensive care units (NICUs).
Rapid and accurate detection of resistant microbes could help to prevent new infections in this setting. To this end, in a pilot study slated to begin in December 2024 and funded by EPIC’s Ignite Grant program, Fralick and his cross disciplinary team of scientists, neonatologists and clinicians will apply environmental surveillance- swabbing hospital surfaces at Mount Sinai’s NICU, including the floors and incubators, and using molecular biology and genomic technologies to monitor the emergence of AMR.
According to Fralick, who received a 2024 Gairdner New Investigator Award, environmental surveillance has the potential to provide clinicians with near real time information about where the AMR bacteria are originating, including very specific information such as the room or the incubator where the resistant strains are first observed, and the antibiotic resistance mechanisms present in the strains.
“Knowing what antibiotic to select for hospital acquired infections is often driven by a hospital’s antibiogram,” said Fralick. Antibiograms are charts generated by the diagnostic microbiology lab that outline the different microbes present in the hospital and their antibiotic sensitivities. “Antibiograms lag by at least one year and they are not specific to an individual area of the hospital such as the NICU. Our study will determine if environmental surveillance might provide real time data to help inform antibiotic prescribing,” said Fralick.
Delving deeper
Alongside environmental surveillance of hospital systems, EPIC members are drilling deeper and investigating the biological processes by which bacteria develop AMR.
In a project partly funded by the EPIC Doctoral Awards program, Viplav Agarwal, a PhD student in Marcus Dillon’s laboratory in UTM’s department of biology, looks at the impact of bacterial population sizes on the development of antibiotic resistance in E. coli.
“At higher population sizes, bacteria accumulate genetic mutations associated with antibiotic resistance,” said Agarwal. These mutations are often present in a bacterial gene that codes for an enzyme essential for DNA replication. When bacterial cells divide, they need to make a copy of their DNA to pass on to their daughter cells. Ciprofloxacin, the antibiotic used in this study binds to the enzyme and inhibits the process by which bacteria duplicate their DNA. The mutations observed by the Dillon lab allow the bacteria to bypass this inhibition.
“Antimicrobial resistance evolves relatively quickly, typically within a few years after the introduction of a new antibiotic,” said Dillon. “Our laboratory experiments help inform clinicians what the evolutionary mechanisms of AMR resistance are, identify genes for surveillance efforts and antimicrobials for treating different types of infections.”
AMR provides bacteria with very a specific advantage- overcoming the antibiotic pressure. However, the acquisition of resistance often requires an adaptation that reduces a microbe’s ability to grow and compete in the absence of those antibiotics.
“Neisseria gonorrhoeae exists only in humans and has a unique evolutionary relationship with AMR,” said Duncan Carruthers-Lay, recipient of an EPIC Doctoral Award and a PhD student who is jointly supervised by Scott Gray-Owen, academic director of EPIC, and John Parkinson, senior scientist at the Hospital for Sick Children (SickKids). Both Gray-Owen and Parkinson are professors of molecular genetics at Temerty Medicine.
Neisseria gonorrhoeae is the bacteria that every year causes over 82 million cases of gonorrhoeae, a sexually transmitted disease. Antibiotic treatments vary between countries, and this changes the profile of antibiotic resistance genes in N. gonorrhoeae isolates found across the world. In North America and Europe, where penicillin and tetracycline are not prescribed for this infection, the bacteria are less likely to carry the resistance genes for these antibiotics. In contrast, in Asia and Africa, where these antibiotics are prescribed, the bacteria retain these resistance genes.
“The mutations allow bacteria to survive the antibiotic pressure, but they don’t hold on to them if they are not useful because they carry some downsides,” said Carruthers-Lay to explain why bacterial populations lose resistance genes. “If we understand the downsides, we can begin to add additional pressures to counter the AMR advantages developed by these bacteria.”
Using nature against nature
Expanding on the idea of understanding bacterial biology to overcome AMR, Véronique Taylor, recipient of EPIC’s Career Transition Awards and a research associate in Karen Maxwell’s laboratory in U of T’s department of biochemistry, studies bacteriophage that target the bacteria Pseudomonas aeruginosa, a common cause of hospital acquired infections. Bacteriophages, or phages, are viruses that attack bacteria and are being tested as a possible line of treatment for drug resistant infections.
“The bacteria have evolved upwards of about 20 different types of anti-phage defence systems to protect themselves against viral attacks,” said Taylor. “To take the next step and make phages capable of infecting any kind of hospital acquired or AMR bacteria, we have to understand the conditions under which the defences are activated.”
The Maxwell research group has developed a fluorescence-based reporter assay to study which defence mechanisms are activated under which conditions. This information can be used to engineer phages that can bypass the defence mechanisms present in AMR bacteria. “Phages naturally predate bacteria, making them an exciting strategy to neutralize AMR strains,” said Taylor.
“AMR has the potential to once again make common infections life-threatening,” said Gray-Owen. “Each case is different, so EPIC researchers are working to confront this emerging threat by developing a suite of innovative new approaches that can be implemented in different scenarios, which should allow us all to breathe easier.”