Results of the 2024 Convergence Postdoctoral Fellowships Competition
The Emerging and Pandemic Infections Consortium (EPIC) is an integrated network for researchers, trainees and partners working to confront infectious disease challenges. We unite members across the University of Toronto and its hospital partners to accelerate cross-disciplinary work in the understanding and development of new countermeasures against pathogens. A key pillar of EPIC’s work is training the next generation of infectious disease research leaders that will help stop future pandemics and reduce the societal burdens of infectious disease.
EPIC Convergence Postdoctoral Fellowships support postdoctoral trainees who are driving innovative infectious disease-focused projects that bridge two research disciplines. These senior trainees are expected to engage faculty from at least two different departments and/or divisions, with formal co-supervision by each. By linking together expertise from different research areas, EPIC Convergence Postdoctoral Fellowships will help strengthen the connectedness and interdisciplinarity of EPIC’s research community while advancing leading-edge research.
We are pleased to share the results of our 2024 Convergence Postdoctoral Fellowships competition, which included a special funding call for the Pfizer EPIC Convergence Postdoctoral Fellowship in Vaccinology.
Total investment
Meet our 2024 Convergence Postdoctoral Fellowship recipients

Guillaume Dugied
Department of Molecular Genetics, Temerty Faculty of Medicine
Supervisors: Mikko Taipale (University of Toronto, Temerty Faculty of Medicine) and Laurence Pelletier (Lunenfeld-Tanenbaum Research Institute)
Project title: Identification of pathogenic effectors inducing cellular morphological changes
Project summary
Infectious diseases are caused by human pathogens such as viruses, bacteria, and parasites. Pathogens live at the expense of their host by modulating the cellular environment to favour their replication during the course of infection. To do so, pathogens use proteins called effectors that play a central role in the remodelling of the host cell environment. While remodelling the host cell environment, these pathogenic effectors often affect the morphology of the host cells. Although there are ~1,400 human pathogens, our understanding of pathogenic effectors is mostly based on a small number of well-known pathogens. Thus, there is a great need to characterize pathogenic effectors. Poor characterization of pathogenic effectors derives from the need for more technology capable of capturing more than one perturbation at a time, and the absence of a large collection referencing thousands of pathogenic effectors. To resolve this issue and characterize the role of pathogenic effectors, we generated a collection containing over 6000 pathogenic effectors. Additionally, I will use a multidisciplinary approach combining functional genomics, microscopy and my background in infectious diseases to provide critical insights into pathogenic effector functions. I will establish optical pooled screens, a technology using high-content imaging followed by in situ sequencing to associate cell morphological phenotypes to pathogenic effectors. This enables the comparative study of different pathogenic effectors, with the goal of clustering them based on their functions. By better understanding pathogenic effectors, we will gain insights into the replication mechanisms of pathogens, and potentially identify targets for the development of therapeutics.

Amin Ektesabi
Unity Health Toronto
Supervisors: Claudia dos Santos (Unity Health Toronto) and Gilbert Walker (University of Toronto, Faculty of Arts and Science)
Project title: Creation of precision miRNA-based therapy for SARS-CoV-2-induced cardiac dysfunction
Project summary
COVID-19 is a severe condition for vulnerable patients, especially concerning how it can affect the heart, leading to serious conditions such as heart failure. About 10% of people who catch COVID-19 experience heart problems, and there’s also a small chance that COVID-19 vaccines might trigger myocarditis. We explore new ways to treat these heart issues, focusing on something called microRNAs. These molecules help control which genes are turned on or off in our bodies and could be key to managing heart problems caused by COVID-19 or, in rare cases, by the vaccine.
We have pinpointed a specific microRNA, miR-187a-3p, that looks promising for protecting the heart against damage from COVID-19. This microRNA can alleviate heart inflammation, which is crucial because inflammation can lead to serious heart damage. Early studies have shown that introducing more miR-187a-3p into the body can lessen heart inflammation and even reduce the risk of death in animal models.
To assure correct bio-distribution, we are using lipid particles, similar to what’s used in some COVID-19 vaccines. These particles can safely deliver miR-187a-3p into heart cells. The hope is that this treatment will not only help the heart function after COVID-19 but also explore how it might protect the heart from potential vaccine side effects. By understanding how microRNAs like miR-187a-3p work, we aim to find better ways to treat or prevent heart problems related to COVID-19, making our fight against the virus a bit easier.

Conrad Izydorczyk
Lunenfeld-Tanenbaum Research Isntitute
Supervisors: Allison McGeer (Lunenfeld-Tanenbaum Research Institute) and Julianne Kus (Public Health Ontario)
Project title: Antifungal resistance and epidemiology of InvaSivE infections due to non-albicans Candida species (ARISE)
Project summary
Antimicrobial resistance (AMR) is estimated to have cost Canada’s healthcare sector over $1B in 2018 and contributed to 14,000 deaths. While the impact of AMR in bacterial infections has long been recognized, it has remained largely overlooked in fungi. This is partly due to a lack of data regarding the burden, epidemiology, and mechanisms of resistance of antifungal resistant infections. Candida species are among the most important fungi causing antifungal resistant infections today. Recent studies suggest that resistance to frontline antifungal agents used to treat Candida infections is increasing globally, especially among non-albicans Candida species (NACS). In order to develop a plan for controlling resistance in NACS, however, an understanding of the risk factors associated with antifungal resistance in NACS infections is required. Similarly, to prevent the spread of these infections, risk factors for infection transmission must be identified.
This proposed project has the specific aims of identifying risk factors for antifungal resistant NACS infections and for acquisition of NACS by transmission events. This will be achieved by combining conventional mycology and susceptibility testing, epidemiology, and bioinformatics/genomics. The results of this project will provide the necessary background for future inclusion of Candida infections in Canada’s action plans to combat AMR. Our team consists of experts in population-scale epidemiology, clinical mycology, and microbial genomics, making us the ideal candidates for this study

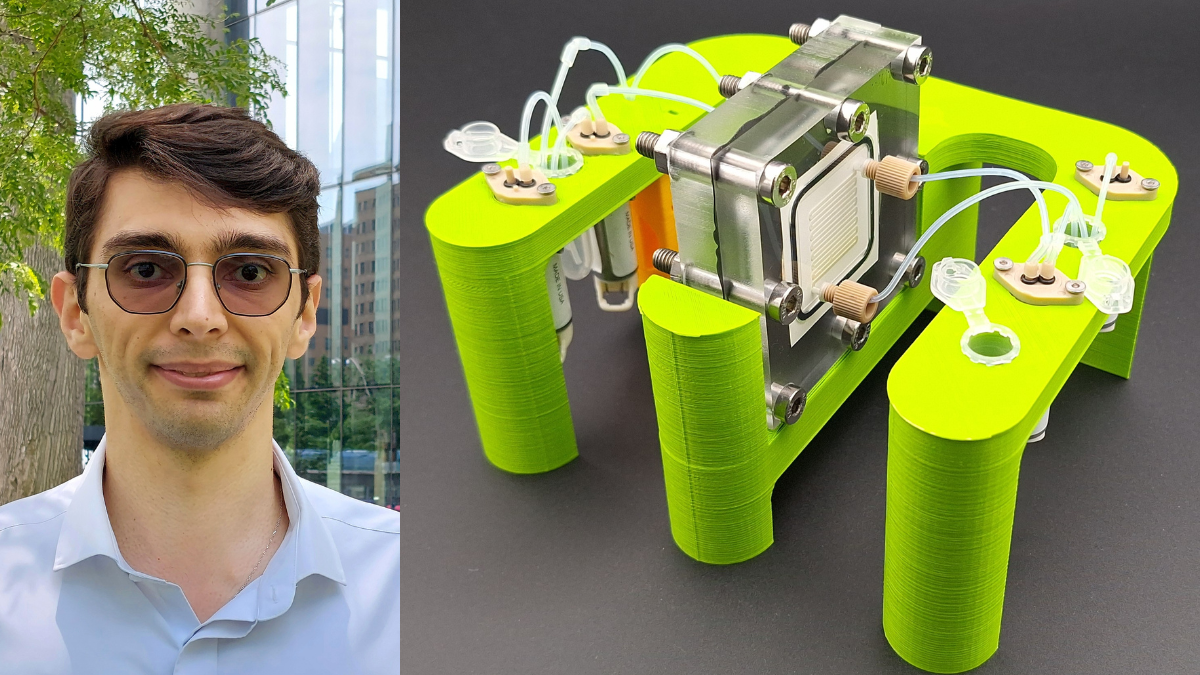
Mohammad Simchi
Leslie Dan Faculty of Pharmacy
Recipient of the Pfizer EPIC Convergence Postdoctoral Fellowship in Vaccinology
Supervisors: Keith Pardee (University of Toronto, Leslie Dan Faculty of Pharmacy) and David Sinton (University of Toronto, Faculty of Applied Science and Engineering)
Project title: Scalable high-yield biomanufacturing for on-demand vaccine production
Project summary
Presently, vaccines are mostly manufactured and distributed globally from centralized foundries, relying on a cold supply chain. This strategy restricts equitable vaccine access in developing and remote regions and struggles to meet high demand during pandemics. My research aims to create a portable, automated device for decentralized vaccine production to cut the reliance on the cold supply chain and facilitate vaccine distribution globally. I propose using cell-free systems, i.e. extracting vaccine production machinery from cells, that can be freeze-dried for room temperature storage, making them more accessible. However, current systems have limitations such as low production yield and the need for specialized equipment and expertise for purification. Our interdisciplinary project aims to overcome these challenges by developing an automated system that efficiently produces and purifies vaccines without specialized knowledge. With the press of a button, users can initiate the vaccine production cycle and have the vaccine ready for injection upon completion. The work will leverage research capabilities in microfluidics and exchange-membrane-based systems in the Sinton lab, and cell-free synthetic biology expertise in the Pardee lab. Having proficiency in electrical and mechanical engineering and expertise in cell-free systems, I will bridge these research groups to form a fruitful, multidisciplinary collaboration. We will use the system to produce protein vaccines for SARS-CoV-2, Ebola, and Crimean-Congo hemorrhagic fever viruses that are WHO priority pathogens. This technology has the potential to revolutionize vaccine distribution, particularly in developing regions, and improve global health security by ensuring rapid access to lifesaving vaccines during pandemics and outbreaks.